A PCOS Problem Is the Presence of Hypothyroidism
On this page, we'll talk about symptoms and causes of hypothyroidism in relation to PCOS, and briefly review Hashimoto's disease.
Free PCOS Newsletter
What Are the Symptoms of Low Thyroid Function?
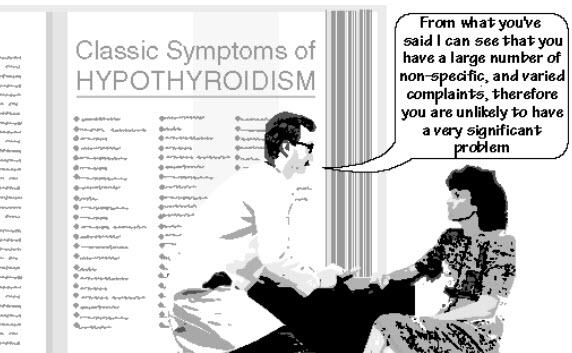
Women with low thyroid function also are more likely to have:
- Acanthosis nigricans (velvety, hyperpigmented skin folds)
- Brittle nails
- Cold extremities
- Constipation
- Depression
- Diabetes - either Type 1 or Type 2
- Dry skin
- Estrogen dominance
- Fatigue or weakness
- Hair loss
- Higher cholesterol
- Inability to focus
- Increased testosterone and luteinizing hormone (LH)
- Infertility
- Insulin resistance
- Lack of ovulation
- Lower body temperature
- Menstrual problems
- Metabolic syndrome
- Muscle aches and musculoskeletal problems
- Ovarian cysts
- Weight gain or inability to lose weight.
What Are Some Causes of Hypothyroidism?
Here are four basic possible reasons for underactive thyroid hormone activity:
- The brain can under-instruct the pituitary, thus causing TSH (thyroid stimulating hormone) to be under-produced.
- The thyroid can fail to make enough T4.
- T4 can be under-converted to T3 in the body.
- T4 can be converted into excessive amounts of rT3, thus partially blocking the cell stimulation of regular T3.
Contributory factors that might cause any of the above four problems include:
- Autoimmune thyroiditis (inflammation of the thyroid gland -- "Hashimoto's Disease")
- Dietary deficiencies
- Exposure to toxic heavy metals
- Exposure to toxic or hormone-disrupting environmental chemicals
- Hormone therapy
- Maternal exposure to environmental chemicals and heavy metals while you were a fetus
- Severe calorie restriction
- Some medications
- Stress
- Thyroid surgery or radiation.
Link between Hashimoto's Disease and PCOS
A medical study was recently published that showed a relationship between polycystic ovarian syndrome and Hashimoto's Disease, which is autoimmune thyroiditis. Autoimmune thyroiditis is an inflammatory condition where your immune system attacks and damages your thyroid gland.
The purpose of this multicenter study was to investigate the prevalence of autoimmune thyroiditis in women with polycystic ovarian syndrome. There were 175 women with polycystic ovarian syndrome and 168 women who did not have this disease in the study. All of the women had extensive lab work.
The PCOS patients were characterized by an increased LH/FSH ratio, low progesterone, elevated testosterone and a high prevalence of hirsutism, but no differences in estrogen levels were found. In addition, 27% of the polycystic ovary women had elevated thyroid-specific antibodies as compared to only 8.3% of the normal women. Elevated antibodies suggest an aroused immune system that is causing inflammation.
Thyroid ultrasound showed that 42.3% of PCOS women, but only 6.5% of the controls, had thyroid tissue images typical of autoimmune thyroiditis (Hashimoto's Disease).
The PCOS women also had higher levels of TSH (thyroid stimulating hormone) than the other women, suggesting that the PCOS thyroid is not as successful in making enough thyroid hormone.
The importance of the thyroid hormone for the adequate functioning of multiple organ systems within the body cannot be overstated. The production of adequate quantities of thyroid hormones is necessary for normal fetal and neonatal growth and development, as well as proper functioning of adult organ systems, cardiovascular system, lipid and carbohydrate metabolism, and the neuromuscular and skeletal systems.
Bottom Line: This study suggests that 4 of every 10 women with polycystic ovary syndrome probably have impaired thyroid function, due to autoimmune thyroiditis (Hashimoto's Disease). Therefore, an important component of your treatment is to get a thorough thyroid evaluation from your doctor. As we've said before, just taking birth control pills is not the complete answer to your symptoms.
Related Articles
Sources:
Janssen, OE et al, High prevalence of autoimmune thyroiditis in patients with polycystic ovary syndrome, Eur J Endocrinol. 2004 Mar;150(3):363-9
Su PH et al. Thyroid and growth hormone concentrations in 8-year-old children exposed in utero to dioxins and polychlorinated biphenyls. J Toxicol Sci. 2015 Jun;40(3):309-19.
Du D et al. The relationship between thyroiditis and polycystic ovary syndrome: a meta-analysis. Int J Clin Exp Med. 2013 Oct 25;6(10):880-9.
Singla R et al. Thyroid disorders and polycystic ovary syndrome: An emerging relationship. Indian J Endocrinol Metab. 2015 Jan-Feb;19(1):25-9.
Get Answers to your Questions about
- Fertility
- Weight Control
- Hair Loss
- Stress
- Unwanted Hair
- Acne...and more!
FREE PCOS Report
and Newsletter
Your email is safe with us. We respect your privacy, and you may unsubscribe at any time.
Recent Articles
-
PCOS Long Journey to The Happy End
Apr 30, 18 07:24 PM
Hi Girls, Maybe my story will have one day a good end but I am not there yet. Until I was 31 years old I lived my dream, having lovely husband, good -
PCOS and Miscarriage
Apr 17, 18 04:03 PM
Proper diet and natural supplements can help the body maintain a pregnancy through successful delivery.
-
How to Deal with PCOS and Stress
Apr 04, 18 04:19 PM
Your body has a natural capacity to heal itself if you provide it with the necessary tools.